May 7, 2019
Five Reasons You Need Patient Segmentation

Patient segmentation can take many forms depending on the diversity of your patient population and the needs of your organization. The more advanced your segmentation capabilities, the more personal you can get with communications, and the more likely your consumers will take desired actions.
From basic demographic profiling (applying accepted generalizations to patient populations based on what we know about their demographics) to the more advanced predictive modeling (e.g., propensity-to-pay scoring), all types of segmentation work toward one end goal: to build meaningful behavioral consumer profiles for every patient so you know exactly how, when, and where to reach them.
Five Reasons You Need Patient Segmentation
1. It’s a Vital First Step to Customized Patient Communication
You can’t tailor your patient communications if you don’t know the specifics about your patients, who they are, what they like, and how they pay.
Using propensity-to-pay modeling as an example, you can segment your patient population into three pay groups: high propensity, medium propensity, and low propensity. You can then build communication outreach workflows for each segment based on their needs.
The high propensity group is relatively low touch, so the required statements should suffice.
You can further segment the medium propensity group based on the amount of their balance to define the messaging they need, the amount and types of touches required, and offers for payment plans or discounts.
The low propensity group can also be relatively low touch since you know the likelihood of receiving payment is minimal. Instead of spending time and resources reaching out to these individuals, you can more effectively screen for Medicaid eligibility up front or assign a financial counselor to get the best possible outcome from these patients faster.
2. To Earn Stronger Patient Engagement
With targeted, personalized messaging sent via the channels each patient prefers, healthcare organizations can expect to see a boost in patient engagement metrics. What should you measure when it comes to billing engagement? Start with:
- Self-service payments (online and IVR)
- IVR calls resulting in payment
- Payments made in full
- Average days from first statement to payment
- Number of touches before payment
3. It’s the Backbone for Back-end Data Analytics
Public records data can only take you so far in your quest to enhance patient engagement and improve collections. Patient segmentation and behavioral analysis will help your health system link known demographic trends to individual consumer behaviors and preferences to build a meaningful consumer profile that informs future communications and billing decisions.
This type of profiling is then fed into proprietary algorithms to derive predictive scores that in turn feed into decision-making workflows and business intelligence models to continually improve revenue cycle performance and the patient financial experience.
Think of patient segmentation as the force that keeps the revenue generation wheel turning faster and faster.
4. To Free Up Customer Service to Work on More Complex Issues
Healthcare providers now have the technology available to facilitate payments without the assistance of a live customer service professional — something that can be done cheaper and more securely via online payment portals, text-to-pay, and automated inbound voice response (IVR).
With technology doing the legwork and enabling patients to pay without manual assistance, customer service reps have more time to focus on mission-critical service initiatives and give more attention to patients who need complex case management beyond simple payment transactions.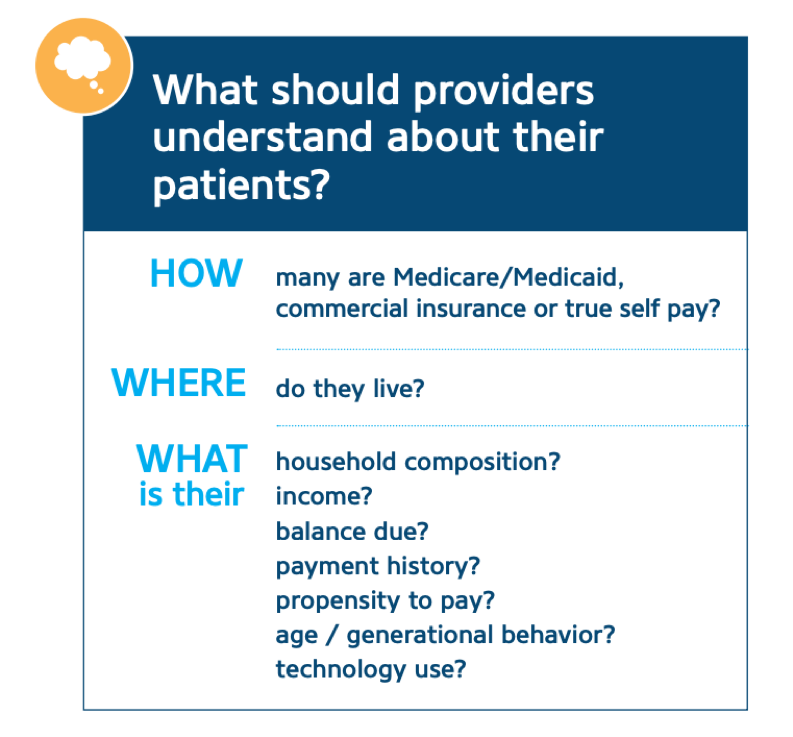
The same health system mentioned above shifted their payment intake flow with the help of patient-facing payment technologies so that twice as much revenue flowed through self-service channels.
5. To Understand Patients as Individuals
Beyond increased revenue and improved patient engagement, the true goal of these patient segmentation and business intelligence efforts is to understand every patient as an individual. Once you do, you can tailor every patient touch point to make the healthcare journey easier, more comfortable, and more productive for all.
When we can predict each patient’s preferences, we can ensure that the financial aspect of their healthcare experience doesn’t detract from their overall wellness.
RevSpring Can Help
Integrated payment communication is part of RevSpring’s DNA. We tailor the payment conversation to influence behavior and inspire action. Our segmentation rules and workflows help you become hyper-focused on the patient, understanding their ability to pay and mapping their financial obligations to repayment pathways.
If you’d like to learn more about our comprehensive patient engagement and billing solutions, we’d love to help you. Request a demo to see how we can help your organization meet its goals.