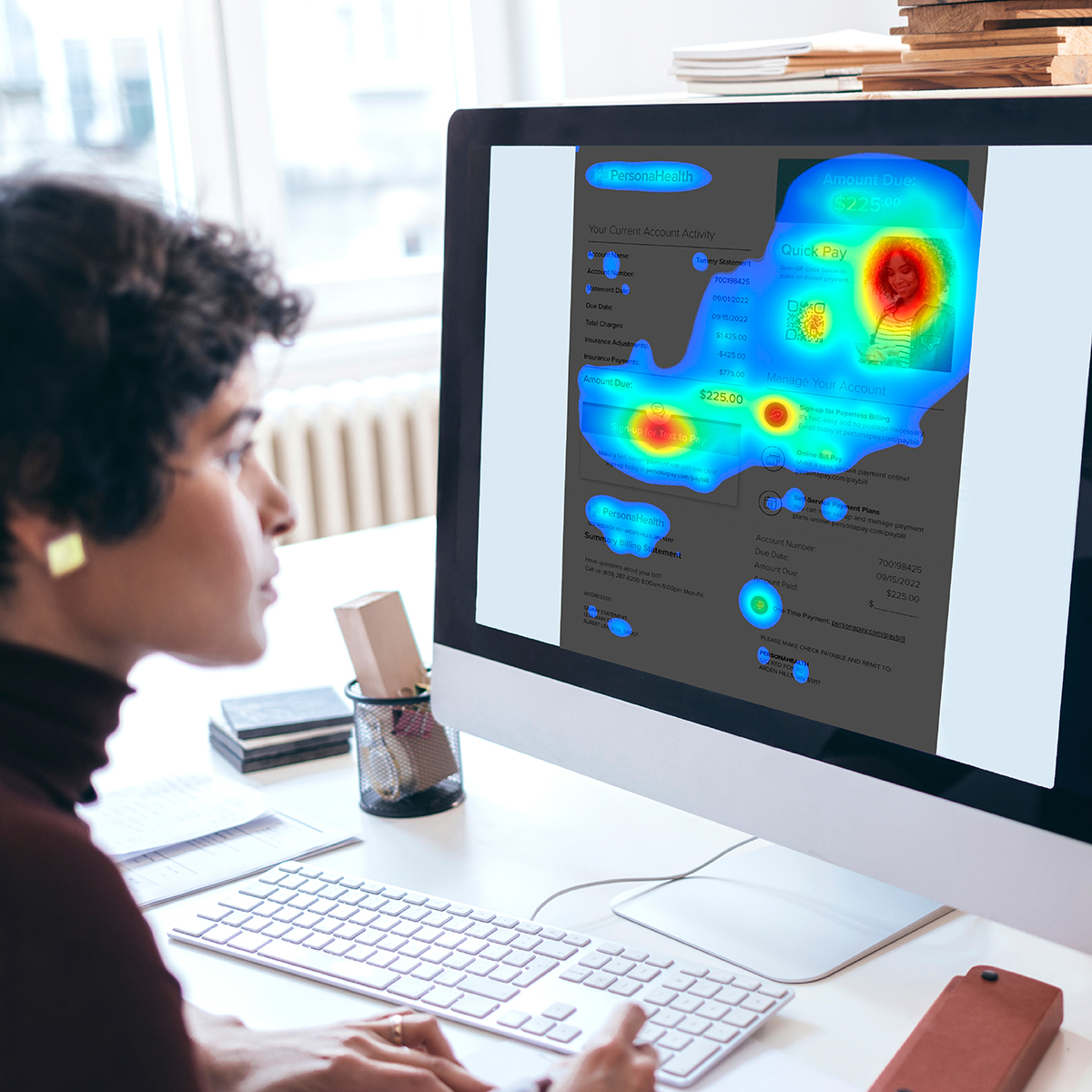
Human Understanding Powered by Intelligence
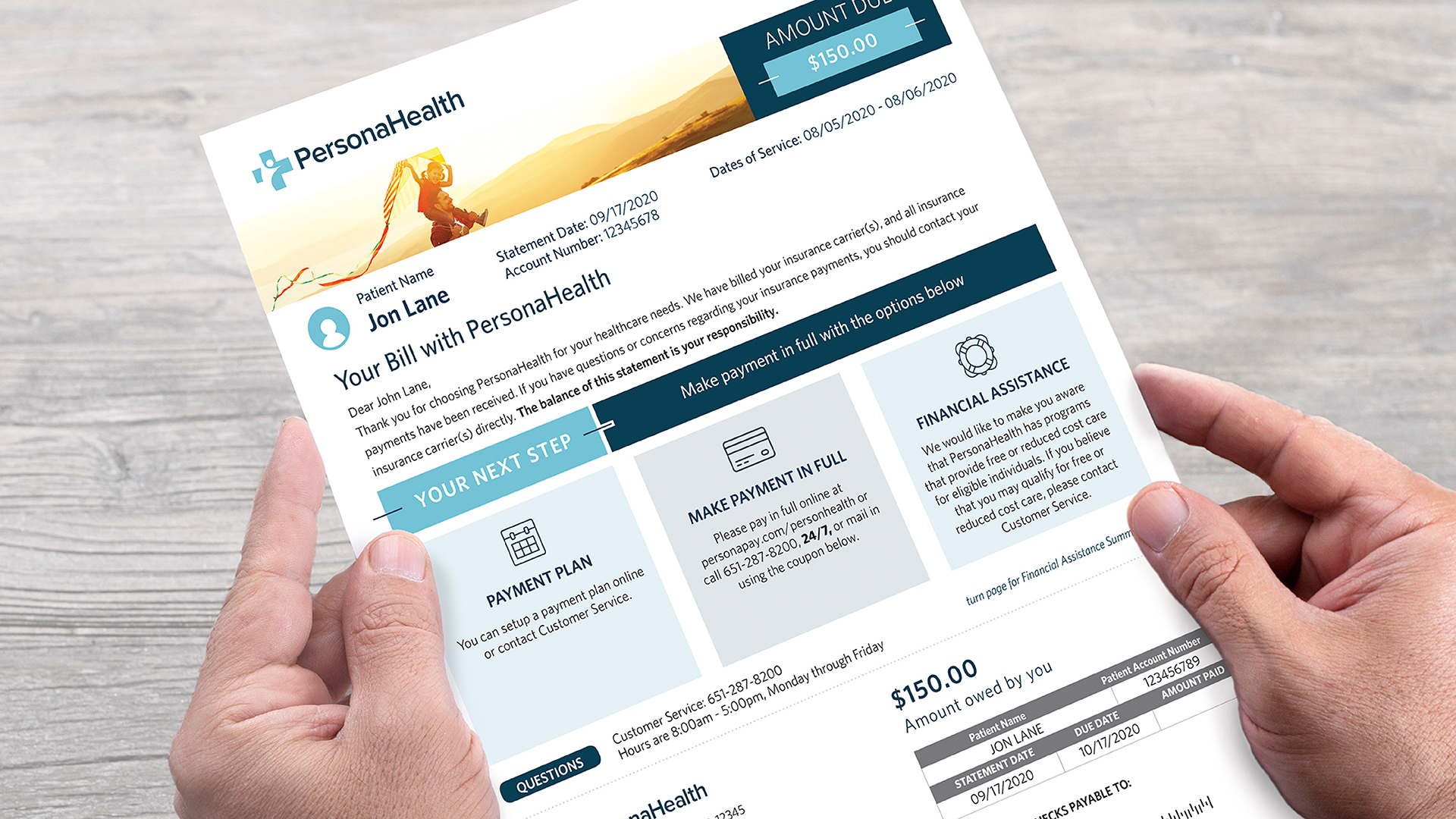
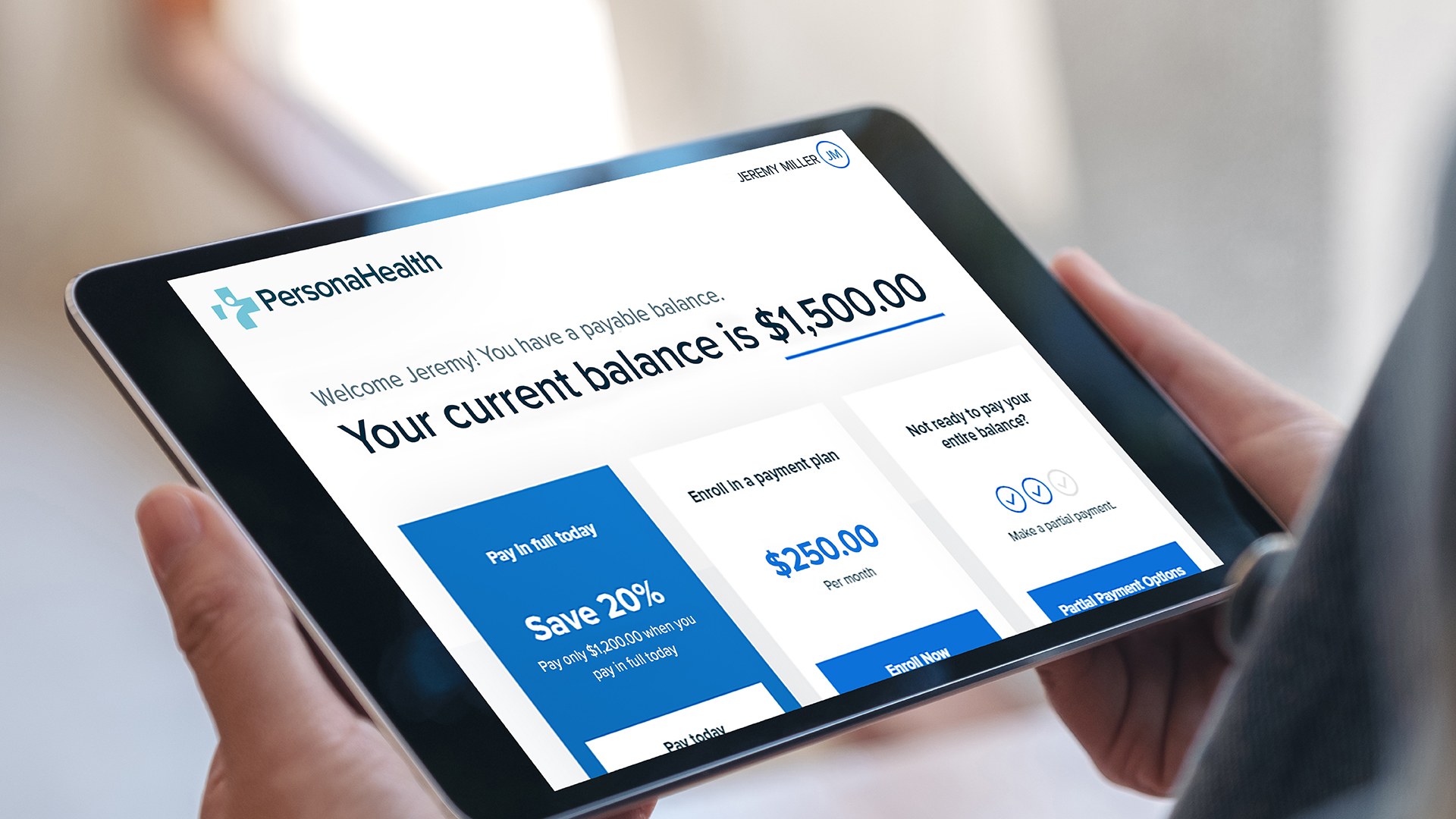
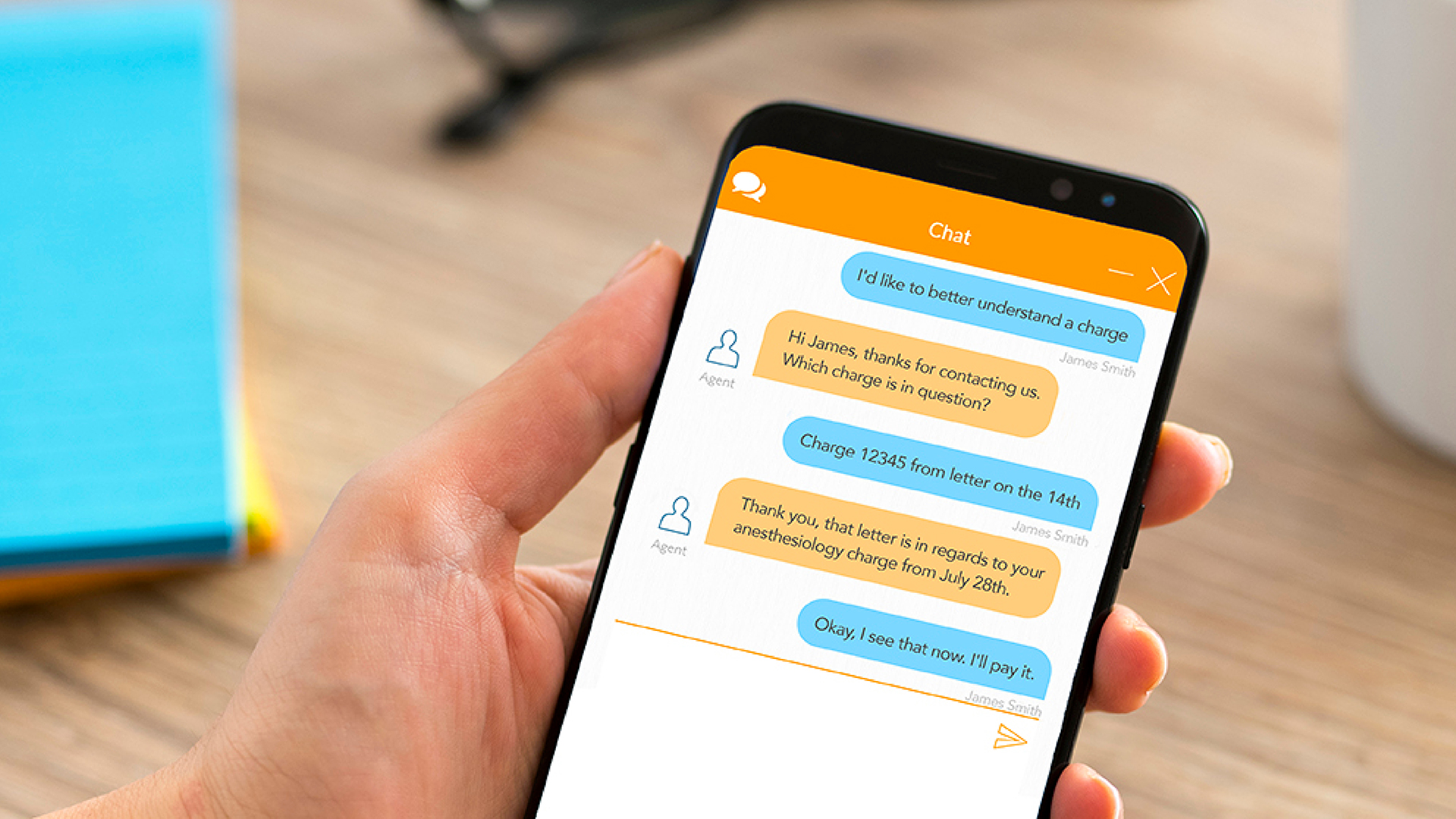
Understanding patients is critical to improving outcomes. Ideally, your patients should feel “they know me” when engaging with you. That’s why we use a propriety approach to analytics to gain more precise insight into your patient’s needs, behaviors and tendencies—throughout their entire healthcare journey. What does this result in? Industry-leading data-based solutions that help healthcare providers find and leverage the most effective ways for patients to resolve their financial obligations, interact with communications, trust their estimates, and more!