June 13, 2018
Strategic Denials Management: The Key to an Efficient Revenue Cycle
Denials are like the check engine light of the revenue cycle. Sure, you can keep rolling for miles with it on, but eventually, you’re going to have to take action. If you’ve ever tested the seriousness of that little dashboard indicator, you know that in some situations the problem is minor. Others, though, can leave you inconvenienced, stranded, or even worse.
Many hospitals and health systems have been sputtering along with that light on just as we’re entering a new era in healthcare. Hospitals are navigating new challenges like value-based care, increasing patient responsibility, and settling into ICD-10, meaning yesterday’s casual warnings from your denials management processes could be signs of tomorrow’s revenue cycle disaster.
This is why now is the time to restart a denials management strategy that preserves revenue and keeps your organization humming.
Getting Reacquainted With Denials
Denials are so common in claims management that, for most of us, they’re just part of the terrain. Today, though, avoiding unnecessary leakage requires a new approach.
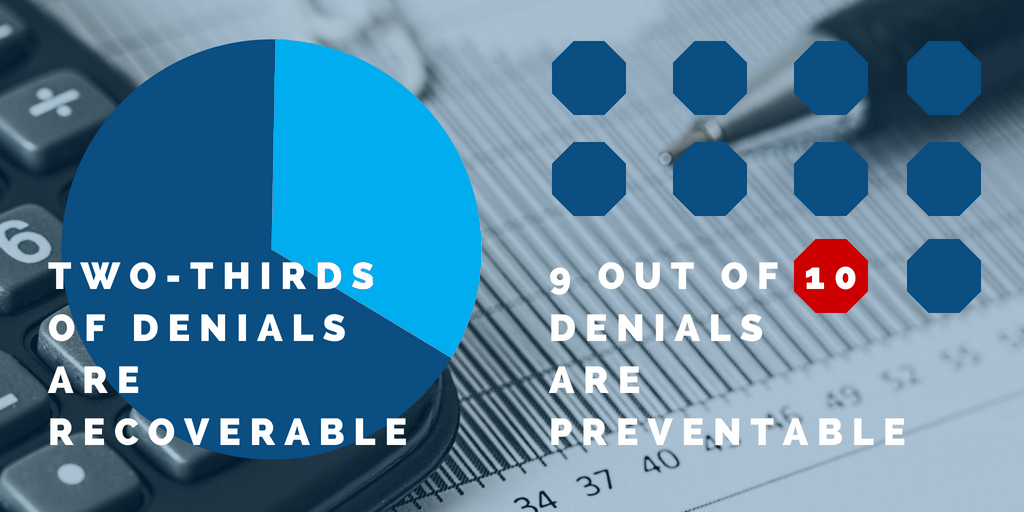
Overall, revenue lost to denials is starting to spike — Eide Bailly cites estimates that gross charges denied by payers has jumped a full 15 to 20 percent, and that’s on top of the fact that as much as 65 percent of denied claims never get worked. This amounts to a denials environment where even efficient facilities can expect the average 3 percent of net revenue lost to denials to start creeping skyward.
That said, the most important numbers involve what’s going on at your facility. Do you have a general idea of how much you lost to denied claims last quarter? What about which direction that number is trending? If not (and honestly even if you do), you probably have room to make real gains — with a few adjustments.
Understanding the Current State of Your Denials
Slowing leakage starts with identifying the top denials in your revenue cycle processes. Some of the most common issues include:
- Missing or incorrect information (like patient demographic information or technical errors on claims)
- Duplicate claims
- Previous adjudications
- Services not covered
- Timely filing issues
A 2014 Advisory Board study found that almost 90 percent of denied claims are preventable, so while the top denials at an individual facility might differ, keep in mind that pinning down your top offenders is always a useful exercise.
Building Strategic Best Practices
A reactive approach to denials is a risky one — remember that you shouldn’t wait until your check engine light comes on to respond. You want to prevent it from showing up in the first place by identifying root causes and taking strategic action.
Your denials management strategy and accompanying best practices should be founded on the specific challenges and requirements of your payer mix and serve as the beginning of a feedback loop that informs future adjustments to your revenue cycle workflows.
Step Away From Reactive Billing
Far too many hospitals and health systems take a wait-and-see approach to denials management. Instead of observing payer guidelines from the beginning, their processes use denials as a primary source of information in directing billing and appeal processes.
Reworking claims might be normal, but it isn’t efficient. The Medical Group Management Association estimates an average cost of $25 to rework a claim, so there’s serious financial incentive to get claims right before they go out the door. This means that a focus on submitting clean claims the first time can pay off quickly — don’t discount the benefits of internal audits and taking the time to calculate (and monitor) your clean claim rate.
Invest in Analytics and Technology
However manual your revenue cycle processes might be, technology can be incredibly effective in getting ahead of denials. Tracking critical KPIs can yield a huge efficiency boost, and the right business analytics will help you dive into your most problematic reason codes as well as develop the metrics that best fit your organizational needs and goals.
The benefits of tech don’t stop there. HIT innovation has given hospital leadership an easily integrated array of tools to efficiently zero in on denials management hurdles.
Prioritize the Front End
Denials don’t exist in a vacuum. They can be the result of anything from bumps in patient registration to a lack of information, or even insufficient biller training, meaning a little attention paid on the front end can go a long way. Some hospitals like Baptist Health South Florida have even seen big benefits from front-end-focused initiatives like letting clinical documentation specialists work with providers to prevent issues related to ICD-10.
Not all front-end fixes have to be low-tech though. Upgraded patient scheduling and registration systems can help catch common denial reasons like incomplete insurance verification or incorrect patient demographic information.
The most important takeaway here is to step away from waiting. Just like that little engine light, warnings in your denials processes that you’ve gotten accustomed to ignoring might be the sign of a very big and very expensive revenue cycle disaster in the future. Listening to your denials and getting ahead of the problem can be the best decision you make for your organization this year.
We know healthcare, and that’s why we put data to work for you and your staff. RevSpring Health is a leader in payment systems that maximize revenue opportunities in acute and ambulatory settings. Our at-a-glance dashboards help hospitals and health systems quickly find and close workflow gaps that are costing time, resources, and hard dollars. Since 1981, RevSpring has built the industry’s most comprehensive and impactful suite of patient engagement, communications, and payment pathways backed by behavior analysis, propensity-to-pay scoring, intelligent design, and user experience best practices.
If you’d like to learn more about our comprehensive patient engagement and billing solutions, we’d love to help you. Request a demo to see how we can help your organization meet its goals or stop by Booth #225 at the HFMA Annual Conference in Las Vegas from June 24-26, 2018.