April 17, 2018
Why Patient Experience Matters With Overall Quality Scores
The CMS announced in November 2017 a new approach to quality measurement in response to continued provider concerns about delivering quality care under the Affordable Care Act’s value-based public approach to patients as consumers of healthcare. The new initiative, called “Meaningful Measures” is designed to measure providers only on those elements of care that they can truly influence.
Logically, this makes sense. About 80% of what impacts patient health happens outside of the provider’s facility. Additionally, primary care physicians who are part of a larger health system have reported that the burden of quality-of-care metrics has led to dissatisfaction and consideration of early retirement.
The CMS, in recent remarks, has heard these concerns and revamped requirements accordingly. The organization is committed to a renewed focus on empowering patients and doctors to make sound decisions about healthcare, make care more innovative and affordable, and improve the CMS customer experience. The new metrics when it comes to quality-of-care now center around six key areas:
- Remaining top on the list is reducing readmission rates and ensuring coordination of care. The new focus in this metric grouping includes medication management designed to reduce drug abuse in patients, as well as a seamless transfer of health information (PHI) between providers.
- Also remaining a top priority is the effective prevention and treatment of chronic disease. These measures are largely unchanged from the prior quality metrics with a few key exceptions. Prevention of opioid use is specifically called out in the new metrics, as well as the management of mental health.
- Community engagement is the third component that is consistent with the last set of quality metrics. Providers must still continue to ensure equity of care across all members of the communities they serve, as well as continue a dialogue and work with community leaders to address public health concerns.
- Making care more affordable is a new metric. Providers are now asked to be more selective or discerning in the use of healthcare services and making sure that use is appropriate. Total cost of care should also be considered from a holistic, patient-focused perspective.
- Case on-site should be made safer by reducing potential harm factors in the delivery of care. This includes healthcare-associated infections and preventable healthcare harm.
- Finally, the last set of metrics involves strengthening person and family engagement to ensure a true partnership between the provider, the patient, and the patient’s support network. This is designed to ensure that care is aligned with patient preferences, including end-of-life care in situations where this is the patient preference.
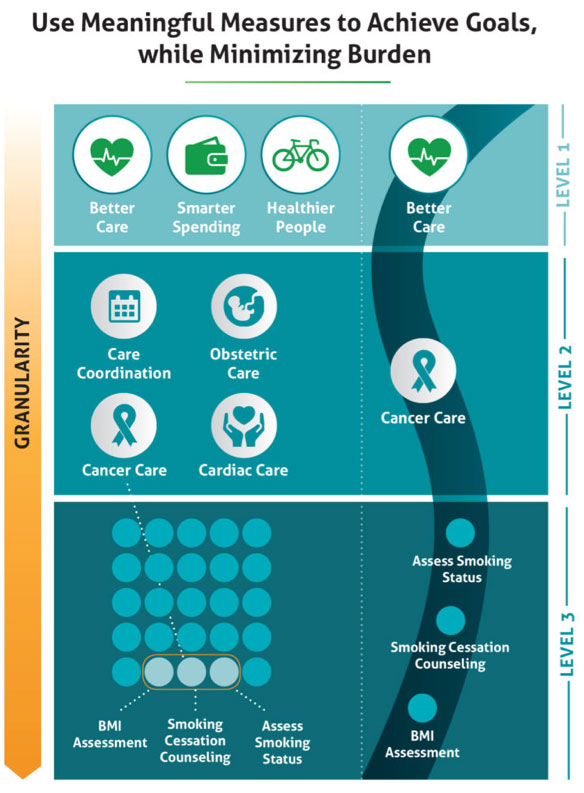
There is also a new approach towards the care episode as part of the larger spectrum of preventing public health issues, as shown in the following example about smoking cessation.
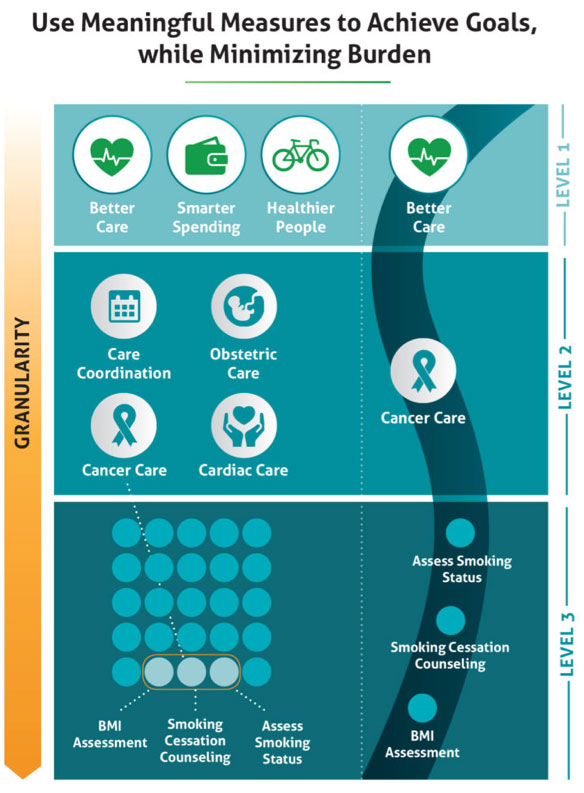 This illustration demonstrates the need to move away from linear thinking (that there’s only one stimulus for every effect) and shift toward an understanding of how risky or unhealthy behaviors are environmental and not situational to the episode of care. Providers must now show how behaviors impact the total health of a patient and not just focusing on one example such as cancer prevention through smoking cessation (example in the diagram). For a female patient, for example, smoking cessation can include cardiac care, obstetric care, and coordination with other potential care providers such as personal trainers or physical therapy.
This illustration demonstrates the need to move away from linear thinking (that there’s only one stimulus for every effect) and shift toward an understanding of how risky or unhealthy behaviors are environmental and not situational to the episode of care. Providers must now show how behaviors impact the total health of a patient and not just focusing on one example such as cancer prevention through smoking cessation (example in the diagram). For a female patient, for example, smoking cessation can include cardiac care, obstetric care, and coordination with other potential care providers such as personal trainers or physical therapy.
Better care is the goal – but it goes beyond better care in the new CMS guidelines. Providers must also demonstrate smarter spending, as well as healthier people. This shift not only incorporates great quality and service but now includes point of care and elevating the conversation of health to the daily lives of the communities that providers serve.
What does this mean for hospital executives? A renewed focus on patient education as the most likely outcome – if patient empowerment is at the cornerstone of these quality metric changes, then providers must do what they can to make sure patients are as informed as possible about how their whole environment and habits at home and work can play into their health outcomes.
These changes would also suggest that hospital administrators must have technology solutions in place above and beyond basic patient portals to help prepare and continue to engage patients throughout their entire course of care. Current patient portals tied to HIS are not user friendly and do not follow best practices for a positive user experience. We expect to see significant upgrades to patient portals to meet the upcoming demand for better patient communication in light of these quality metric changes.
Quality metrics around affordability of care are especially noteworthy, since they open up significant opportunities for patient communication throughout the entire billing experience. This encompasses giving patients a better idea for total out-of-pocket costs before services are rendered, as well as clearly communicating financial responsibility and payment options. Additionally, any patient communication must be mobile friendly, as the need for consistent communication and the ability to reach patients must meet the demands of the 24/7 mobile culture we have become.
To learn more about how you can incorporate a mobile friendly and a 360-degree patient communication program that stays with the patient throughout the entire billing experience, contact RevSpring today. Request a demo to see how our comprehensive patient engagement and billing solutions can help your organization meet your goals, or connect with us on Twitter, LinkedIn, or Facebook to learn more.