April 10, 2018
What Defines a Quality Patient Experience?
A 2017 National Bureau of Economic Research study examined statistical relationships between common HCAHPS quality metrics and looked at how these metrics accurately predicted objective measures of quality care, such as lower mortality rates and lower readmission rates.
The headline? The only two metrics that truly impacted lower mortality rates or lower readmission rates involved patient satisfaction. According to the study’s findings, the CMS metrics accurately predicted readmission, 30-day mortality, and 365-day mortality when all inputs were entered into a regression model.
The following measures were evaluated in the study:
- Process measures: this quantifies the provider’s ability to deliver timely and effective care. Metrics in this cluster came from the CMS and National Quality Forum’s Hospital Compare program, the Leapfrog Group, and the U.S. News and World Report’s annual hospital rankings.
- Patient experience measures: These were directly taken from HCAHPS survey data.
- Outcome measures: These were dependent variables of readmission and mortality rates reported to CMS.
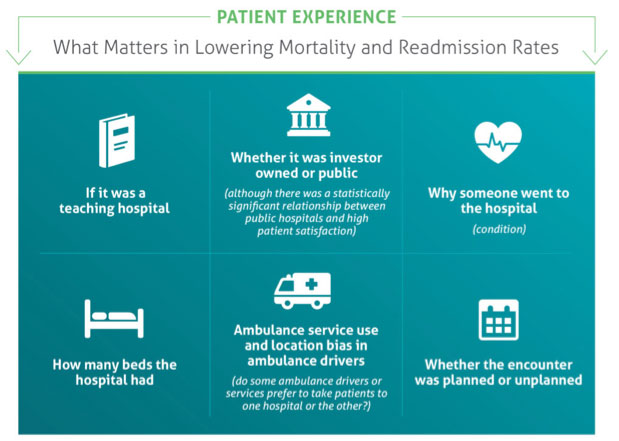
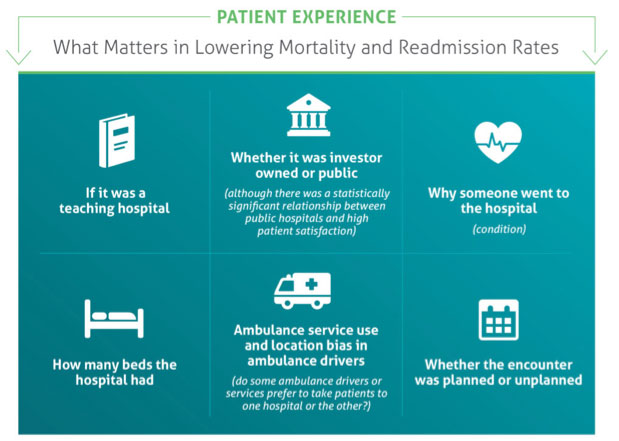
Other quantifiable metrics were included in the study to see if there was a relationship between patient treatment data and other ancillary factors, as well as patient-focused processes and experience metrics. Factors that had no statistical relationship whatsoever to readmission or mortality were:
 So what makes up a great patient experience? Patients receive great communication from doctors and nurses, their pain was always well controlled, responses for help arrived as soon as it was requested, and staff always explained everything. Having clean, quiet rooms was also an important factor in patient satisfaction.
So what makes up a great patient experience? Patients receive great communication from doctors and nurses, their pain was always well controlled, responses for help arrived as soon as it was requested, and staff always explained everything. Having clean, quiet rooms was also an important factor in patient satisfaction.
What can be done to make a positive patient experience, and what’s within a CFO’s control? Continue the patient encounter experience with great communication throughout every touchpoint of the revenue cycle. It is critical to have an intelligent patient payment communications strategy, and ensure patient-centric payment channels. For example, make sure bills are clear and easy to read, as well as offering 24/7 omnichannel payment options.
If you’d like to learn more about our comprehensive patient engagement and billing solutions, we’d love to help you. We can share customer success stories and case studies, and give you the resources you need to choose the right solution for your organization. Request a demo to see how our comprehensive patient engagement and billing solutions can help your organization meet your goals, or connect with us on Twitter, LinkedIn, or Facebook to learn more.