March 14, 2019
Three Ways Healthcare Organizations Improve Self-Pay Processes

It‘s Time to Change the Way You Think about Patient Payments
Innovative revenue cycle management and payment processing companies know that patients engaged throughout the service delivery cycle are more likely to participate fully in billing and payment processes. Healthcare organizations focused on revenue cycle optimization take cues from consumer-focused industries. As a result, revenue cycle workflows are evolving and expanding to put greater focus on pre-service self-pay patient engagement.
Our blog post, “Make Pre-Service Self-Pay Automation a 2018 Priority” explored proactive patient communication as a strategy to help healthcare organizations optimize their revenue cycle and close payment gaps. In this post, we highlight three ways healthcare delivery teams can leverage proactive communication to improve self-pay processes in 2019.
Early Patient Outreach Improves Revenue Cycle Performance
In a survey of senior healthcare finance executives and revenue cycle leaders, researchers at the Healthcare Financial Management Association explore self-pay processes and patient financial engagement efforts. This research confirms that organizations gain significant payment ground when they set financial expectations early in the patient outreach cycle. Full-circle communication and pricing transparency are proving to be the foundations of a strong revenue cycle.
What Can Healthcare Organizations Do to Improve Self-Pay Processes in 2019?
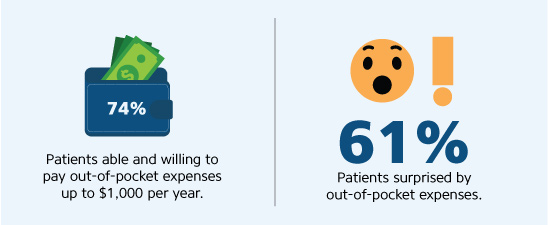
- Avoid acute sticker shock. No one likes an unexpected bill following a visit to the hospital. Yet 61 percent of patients are surprised by their out-of-pocket acute care expenses. Take the surprise out of service costs with improved pre-service patient communication powered by technology.
A comprehensive patient communication platform helps healthcare organizations provide valuable financial information before service is delivered. According to Accenture, patients say that communication is a payment workflow must-have. Nearly half of surveyed patients say they would switch healthcare providers for the ability to understand cost upon scheduling a service appointment.
- Create open communication paths. Bring patients into the payment conversation with focused billing strategies. According to a report from TransUnion, three in four patients report a positive billing experience when an estimate of services is delivered up front. Patients are consumers — they want a consumer-oriented communication experience.Leverage technology and focus on the power of “now” by delivering tailored communication at every touch point. Pre-visit communication delivered through email, text and phone keep the lines of communication open, creating a cohesive and intuitive communication and payment conversation.
Look for intelligent payment communication solutions that provide patient outreach and education at every stage of the care delivery experience. Automated payment communications solutions improve end-to-end patient engagement, increase payments and reduce billing surprises.
Sources: McKinsey, TransUnion
- Leverage business intel to power decision support. Advanced business intelligence solutions show you what to expect from daily, weekly and monthly patient volumes. Harness the power to predict each patient’s impact on your revenue cycle and channel patients to payment solutions that reflect their ability and willingness to pay.Artificial intelligence and business intelligence tools deliver patient insights and guide pre-service and point-of-service billing conversations. Real-time revenue cycle intel helps you guide patients along payment pathways that optimize your revenue cycle.
Patient engagement begins long before the patient arrives in the waiting room; payment conversations should follow suit. Improve the patient experience by focusing on consistent and comprehensive engagement at every touch point. From pre-visit appointment outreach and billing education to point-of-service cost estimation and payment options, leverage technology solutions that break down communication and pre-service payment barriers.
RevSpring Can Help
Integrated payment communication is part of RevSpring’s DNA. We tailor the payment conversation to influence behavior and inspire action. Our segmentation rules and workflows help you become hyper-focused on the patient and their unique payment pathways.
If you’d like to learn more about our comprehensive patient engagement and billing solutions, we’d love to help you. Request a demo to see how we can help your organization meet your goals.