July 18, 2018
Step Into a New Era of Patient Scoring

Effective patient scoring is about to get a lot more valuable to your organization.
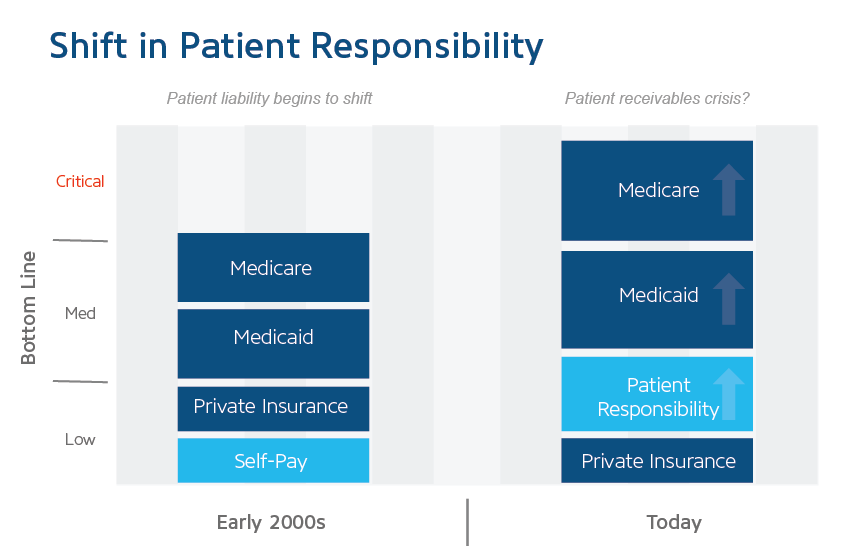
Right now, most hospitals approach patient account scoring by focusing exclusively on either the front or back end, but with patients still showing up as the third-largest payer behind Medicare and Medicaid, a blended approach will likely become a hallmark of a healthy revenue cycle.
 Think about it: if any other payer were sitting in your number three spot, you’d probably be tracking trends from end to end and have a customized communication plan in place to optimize collections. The same approach should apply to self-pay.
Think about it: if any other payer were sitting in your number three spot, you’d probably be tracking trends from end to end and have a customized communication plan in place to optimize collections. The same approach should apply to self-pay.
To get started, you need to understand what scoring should look like in an age where patients are functioning as payers themselves.
The Era of Patients as Payers
First, let’s shift perspective.
Patients aren’t just new payers moving up in the rankings; they’re the most complex payers you’ve ever encountered, who also happen to have the least understanding of their new position. This means the factors that made scoring beneficial in the past are becoming more significant by the day. For example, bumps in registration that might have meant negligible dings to cash flow in the past have likely turned into significant leakage as the self-pay portion of hospital revenue continues to balloon.
Still, there’s another layer to the problem. Just as patients are taking on a larger portion of their responsibility, they’re also navigating a more complex insurance environment as consumers. The relatively straightforward world of insurance coverage has swelled to include HDHPs, HSAs, and ACA plans on top of the rainbow of traditional employer-sponsored options. All of that adds up to a payer who, under any other circumstance, would require an army of special attention.
This is where a new approach to scoring comes in.
Scoring allows you to create order out of the complexity of your patients’ preferences, behaviors, and predicted outcomes. Ideally, you will want to turn all that into analytics-based, targeted payment pathways and an intelligent communication plan that promotes patient payment awareness, increases cash flows, and empowers your patients to become partners in settling their financial obligations.
Why a Blended Approach Is Best
The environment that I’ve just described is one that requires awareness at all points along the revenue cycle. Your approach to patient scoring and communication should take advantage of both front- and back-end strengths to optimize overall insight.
Front-End vs. Back-End Scoring: Benefits and Drawbacks
Scoring your accounts on the front end has definite benefits:
- Faster validation of A/R collectability
- More predictable cash collection
- Useful feedback for your hospital charity policy
- Improved relationship with your care community
- 501(c)(3) compliance
- Reduced effort on the back end
The other side of this coin is that a front-end focus can be an expensive process and might cost you lost potential revenue from individuals who might have coverage or other access to funds.
Back-end scoring wins out on cost, but at the same time, those savings are whittled down by the amount of work your staff has to put in to resolve accounts later in the process that might have dropped out because of payment resolution, insurance payment, or other reasons.
In today’s complex self-pay environment, a combination of the strengths of both approaches is necessary, with the use of targeted patient communication to fill in gaps in education and awareness along the way.
Reinventing Revenue Management and Scoring
If that approach sounds different than what you’re used to, it’s because it is.
Yesterday’s perspective on revenue management (what you’re likely using right now) misses an unprecedented opportunity to engage patients and help them help you smooth out your revenue cycle processes along the way.
A proactive approach to educating and communicating with your patients, the same way you would with Aetna or BCBS, is the first and most important step in optimizing what’s arguably your most important payer relationship.
Where RevSpring Comes In
RevSpring is a leader in patient communication and payment systems that tailor engagement touch points to maximize revenue opportunities in acute and ambulatory settings. We combine dynamic workflows, business intelligence, responsive messaging, and behavioral analytics to tailor engagement opportunities so patients can be more proactive in their healthcare journey — from appointment scheduling to payments.
RevSpring leverages “Best in KLAS” software and services to deliver over 1 billion smart medical communications each year that drive increased patient engagement and payment rates. To learn more about RevSpring, visit www.revspringinc.com/healthcare.