April 3, 2018
Quality as a Metric as It Pertains to the Patient
 In October 2012, hospitals with higher than acceptable readmission rates could suffer financial penalties through lower Medicare reimbursements under the Affordable Care Act. Additionally, the Centers for Medicare and Medicaid Services (CMS) mandated a patient satisfaction survey that was to be given to all patients. The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) was designed to make sure hospital satisfaction metrics were publicly available to all patients and consumers as part of a public government website, and hospitals are publicly ranked based on these surveys with scores from one to 100, with 100 being the best.
In October 2012, hospitals with higher than acceptable readmission rates could suffer financial penalties through lower Medicare reimbursements under the Affordable Care Act. Additionally, the Centers for Medicare and Medicaid Services (CMS) mandated a patient satisfaction survey that was to be given to all patients. The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) was designed to make sure hospital satisfaction metrics were publicly available to all patients and consumers as part of a public government website, and hospitals are publicly ranked based on these surveys with scores from one to 100, with 100 being the best.
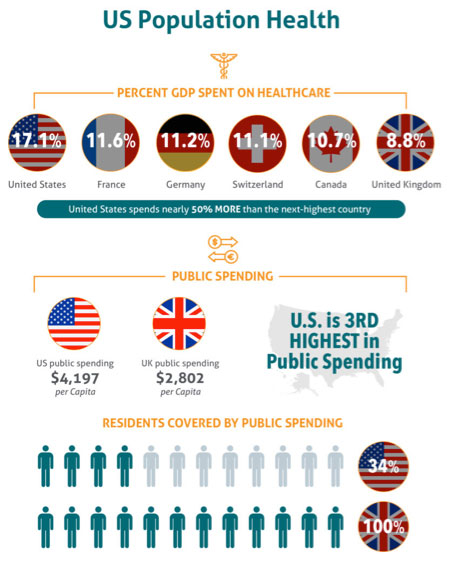
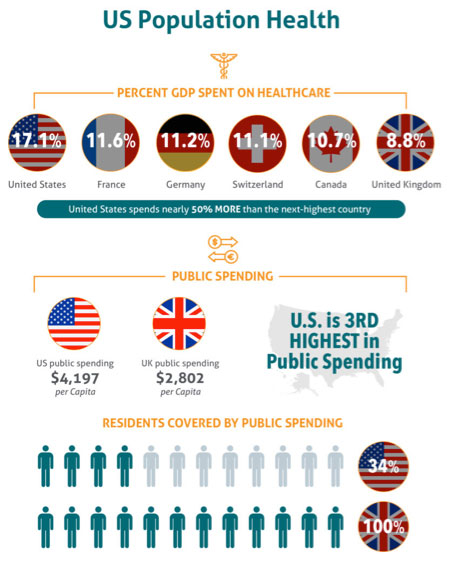
Importantly, HCAHPS scores can impact CMS reimbursements, with the stiffest penalties reducing claims reimbursements up to 2% in cases of exceedingly low HCAHPS scores. It makes sense that the CMS wants to make sure that money goes to providers wisely. The United States spends more on healthcare per capita than any other country in the world, which is interesting considering only 34% of the US population is covered by government healthcare spending.
Challenges of a Standardized Survey
At present, a standardized survey like the HCAHPS survey is the only way to consistently measure hospitals against one another for quality of care. The survey concept may be sound, but its execution remains flawed. Every provider that receives reimbursements from CMS must conduct HCAHPS surveys to a random selection of patients every month and submit results back to the government. These questions involve several key aspects of care:
- Communication with doctors and nurses
- Staff responsiveness
- Hospital cleanliness and other facility-based operational experience metrics
- Pain management and pain management communication
- Discharge information and presentment
- Food services
- Overall hospital rating
 The process has several inherent flaws:
The process has several inherent flaws:
- It assumes that patients are true consumers of their healthcare. Specifically, patients have a pre-existing understanding of how a quality-care experience SHOULD happen and, therefore, are responding to the HCAHPS survey questions from a position of knowledge.
- All patients are randomly selected – meaning that privately insured patients, as well as uninsured patients are in the response population. This can skew the overall results of the hospital’s performance in light of state and national averages based upon the communities that they service.
- This type of methodology creates a disconnect between patient satisfaction and outcomes. For a hospital whose mission is to save lives and to create healthy communities, making a patient well could require processes and procedures the patient doesn’t necessarily like – but are medically necessary. Conversely, a very satisfied patient may be dead in the next year. One study reported that the most satisfied patients had the highest costs, the highest likelihood of hospital admission, and a higher mortality rate than unsatisfied patients.
Flawed as the process may be, it is the only consistent metric in which all hospitals and health systems receiving CMS dollars are measured. Ensuring that patients have a quality-care experience continues to be a top priority, given the direct tie to financial results and its impact on patient-centric payment channels.
A Five-Star System
In April 2017, the CMS changed the way it reported patient satisfaction on its public website to a five-star system. This leverages a quick and easy method for patients to understand the hospital’s rating – like Yelp or Amazon reviews. Hospital administrators have at least 90 days to change procedures to improve their star rating as the CMS ratings are updated quarterly.
CMS has also instituted a compare feature on their website, allowing patients to see ratings across different hospitals in their area and against state and national averages.
How to Improve CMS Ratings
What can hospitals do to improve their ratings? Keep service mentality in mind. Take best practices from other industries such as the hospitality industry. There’s a great case study in the Harvard Business Review that analyzed Cleveland Clinic and how adopting such a change improved service.
Additionally, incorporate RevSpring’s patient engagement strategies that are centered around clear patient communications. RevSpring offers a 360-degree patient engagement experience that delivers comprehensive and consistent communications that begin before the patient encounter and throughout every part of the revenue cycle.
If you’d like to learn more about our comprehensive patient engagement and billing solutions, we’d love to help you. We can share customer success stories and case studies, and give you the resources you need to choose the right solution for your organization. Request a demo to see how our comprehensive patient engagement and billing solutions can help your organization meet your goals, or connect with us on Twitter, LinkedIn, or Facebook to learn more.