June 27, 2024
Knowing Your Patients Is Critical For More Than Caregiving

Product Feature: Analytics
For many healthcare organizations, the patient financial responsibility portion represents the profit margin essential to continued operation. In today’s healthcare, the financial margin, quite literally, is the mission.
In the past, healthcare providers might have been satisfied with sending four patient billing statements within 120 days after an episode of care—the minimum required by federal regulations. This was a solid metric back in the days when 95% of revenue came from insurers. Now, however, with nearly half of patients covered by high deductible health insurance plans,* the goal has shifted.
If this trend of patients bearing a greater responsibility for out-of-pocket expenses goes unrecognized, your organization’s patient payment goals will likely not be met. RevSpring gives healthcare providers the necessary intelligence to fully understand each individual patient’s ability to pay based on key demographic and behavioral data. This not only drives higher yield, it vastly improves the patient experience. Some providers choose to bypass this important step, relying instead on current business rules or protocol. If you’re in that group, we invite you to compare outcomes that providers receive when leveraging RevSpring’s analytics versus those that do not.
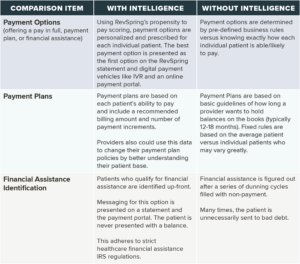
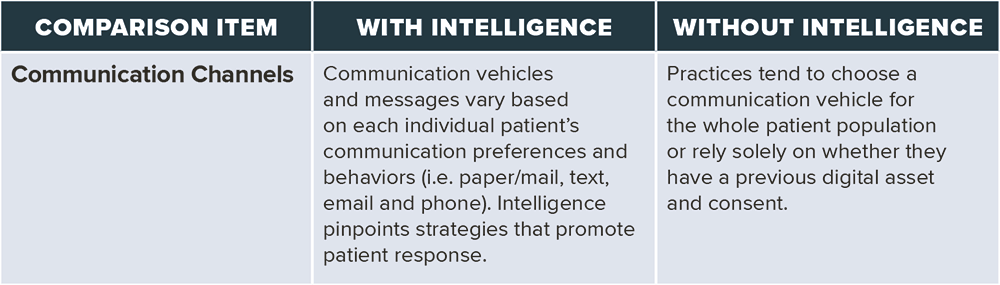
In addition to providing key insights into the patient’s ability to pay, RevSpring also builds in methods for providers to know which communication channel will drive the best response for each individual patient.
Data Doesn’t Lie
Our research reveals tangible results from incorporating intelligence into revenue cycle practices.
- More than 85% of patients will leave a provider after a poor pre-care or billing experience.**A bad billing experience can stem from providers not knowing their patients’ ability to pay and offering unattainable payment options. Using intelligence to understand how each patient is able to pay their financial responsibility demonstrates empathy, which drives a better financial result and greater patient loyalty.
- RevSpring clients using intelligence to determine the right payment option for each individual patient receive payments 25% faster*** within the RevSpring patient portal versus clients not using this strategy.
- RevSpring clients that use payment analytics see a 12% increase in patients choosing the primary payment offer*** because it was driven by the intelligence.
- Clients using payment intelligence see a 5% decrease in abandonment*** on the patient portal because each individual patient is presented with realistic payment options. Patients pay 6.5 days faster from a digital communication.*** Our research also shows that 54% of patients prefer printed bills and statements.** By using intelligence to identify which patients are most likely to respond to a digital communication (email or text), you can accelerate your time to payment for a fairly large segment of your patient base.
Every patient is different. A better patient experience starts with compassion that extends beyond care giver interactions. By matching the right payment options and communication strategy with each patient’s unique needs, patients feel seen and understood. Why guess how a patient is going to respond when you can precisely understand what they can pay, and how they are most inclined to engage?
RevSpring intelligence makes it possible to build this critical insight into every patient interaction. That means you can deliver precisely the right message, at the perfect moment, using the best communication channel, with the most effective financial arrangement to meet each patients’ unique situation and billing obligations. Revenue cycle professionals, in turn, are empowered to improve patient engagement and yield—capturing vital margin— while creating a measurably better patient experience.
Sources:
*US Bureau of Labor Statistics
** RevSpring Voice of the Customer Survey 2023
***RevSpring primary research