June 21, 2018
Connect Patient Billing and the Revenue Stream – Three Tech Fixes

Hospital and health system financial fitness is under fire. Bad debt is plaguing healthcare organizations that once received up to 90 percent of their reimbursement from insurers. Patient responsibility was a small piece of the revenue puzzle and focused on copays and coinsurance, but times have changed.
Patient billing is a necessary and more nuanced component of revenue cycle management, and savvy healthcare organizations know that service billing is only one step along a complex patient engagement journey.
The Changing Face of Payers
According to Ken Kubisty, senior vice president at Advisory Board Consulting and Management, high deductible health plans are changing the patient billing and reimbursement dynamic of healthcare. (For an in-depth look at HDHPs, see our blog series.) Patient responsibility has shifted to nearly 30 percent of the service total. The fundamental reshaping of the reimbursement pie puts greater focus on intelligent, tailored patient billing.
Health systems and patients are in new territory. From insurance coverage and service billing to reimbursement and revenue, everything “health” is changing. For healthcare organizations, tech-powered patient engagement moves the revenue ball forward. Failure to intelligently connect patient communication and billing workflows can result in patient frustration, dissatisfaction, payment delays, and revenue disruption.
Connect on Engagement to Score on Revenue
As in baseball, healthcare teams get several at-bats to connect with patients. Pre-service, point-of-service, and post-service touch points provide valuable opportunities to set payment expectations, answer billing questions, and close financial responsibility gaps.
Patients who are engaged throughout the service delivery cycle are more likely to participate fully in billing and payment processes. According to Accenture, 47 percent of patients would switch healthcare providers for the ability to understand costs up front. That’s a clear signal to healthcare organizations that pre-service billing is top of mind for patients.
Patient satisfaction, billing communication, and revenue are directly connected. The Accenture study also found that 7 percent of patients have switched healthcare providers due to a subpar experience. Dissatisfaction at even single-digit levels adds up, and 7 percent represents more than $100 million in lost annual revenue per hospital.
Leverage Technology to Strengthen Patient Billing Workflow and Revive Revenue
How important is patient billing to the revenue stream? It’s critical, and technology can help healthcare teams predict and often reduce unpaid patient debt. There are three ways that technology tailors patient engagement to keep bill payment responsibility on track.
1) Leverage Predictive Analytics and Machine Learning
Use predictive analytics algorithms to determine the best medium and message for each patient communication. Design print statements with colors, fonts, and layouts that put key details and calls to action front and center. Leverage mobile apps with intuitive navigation that puts user experience best practices to work and at the fingertips of people in your care community. Offer Quick Pay solutions and e-signature options that break down barriers in the payment process and encourage self-service.
2) Rethink and Retune Patient Financial Engagement Workflows
Technology makes painstaking, time-intensive, manual, and repetitive patient finance processes a thing of the past. According to Black Book’s 2017 Revenue Cycle Management survey, 92 percent of hospitals and health systems plan to drop manual back-office billing processes by the end of 2018. Predictive analytics and data-driven decision models bring transparency and ease of use to processing and reconciling medical bills.
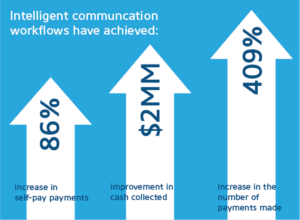 Data-driven patient engagement programs and intelligent communication workflows create tailored payment pathways that net real results. Early adopters of tech-forward solutions have achieved:
Data-driven patient engagement programs and intelligent communication workflows create tailored payment pathways that net real results. Early adopters of tech-forward solutions have achieved:
- A 409 percent increase in the number of payments made
- An increase of 86 percent in self-pay payments
- A $2 million improvement in cash collected
3) Make Electronic Payments a Core Component of Billing and Collection
Bring speed, security, and increased patient satisfaction to your billing and collection processes. When it comes to electronic engagement, consumers have the world at their fingertips. From banking to dinner reservations, consumers expect real-time experiences. The same is true with medical bill payments.
Patients are also consumers, and they want the ability to make payments wherever, whenever, and however their lifestyle dictates. According to Fiserv’s Eighth Annual Billing Household Survey Insights, the quantity and quality of bill pay options are key drivers of customer satisfaction and loyalty. Based on the Accenture report noted earlier in this post, higher satisfaction results in higher on-time bill payment.
RevSpring Can Help
Integrated payment communication is part of RevSpring’s DNA. We tailor patient billing to influence behavior and inspire action. Our predictive analytics and workflows help you become hyper-focused on the patient, understanding the patient’s ability to pay and mapping his or her financial obligations to repayment pathways.
If you’d like to learn more about our comprehensive patient engagement and billing solutions, we’d love to help you. Stop by Booth #225 at the HFMA Annual Conference in Las Vegas from June 24-27, 2018 or request a demo to see how we can help your organization meet its goals.