January 23, 2018
Healthcare Providers to Nix Manual Collection Processes in 2018
 Every health system and medical practice can benefit from keeping a pulse on patient engagement, communications and payment process best practices. Throughout 2018, we will highlight the trends, news and events that impact your competitiveness and bottom line. First up is automation of back-office processes.
Every health system and medical practice can benefit from keeping a pulse on patient engagement, communications and payment process best practices. Throughout 2018, we will highlight the trends, news and events that impact your competitiveness and bottom line. First up is automation of back-office processes.
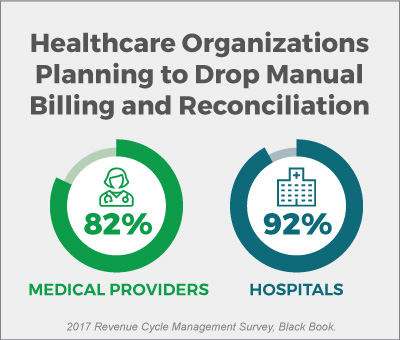
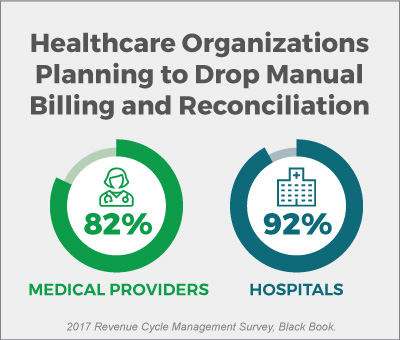
According to Black Book’s 2017 Revenue Cycle Management survey, 82 percent of medical providers and 92 percent of hospitals plan to discontinue “time-intensive, error-prone, manual efforts to back-end process and reconcile bills” by Q4 2018. Black Book gathered data between April 1 and September 30, 2017, from 2,698 healthcare providers, along with 850 healthcare consumers with high-deductible health plans (HDHPs).
Healthcare’s “Perfect Storm” Demands Automation
Several factors are driving the shift away from manual processes in medical billing departments:
- Providers must process and collect more funds directly from patients.
Since 2015, there has been a 29.4 percent increase in the deductible and out-of-pocket costs patients must shoulder. Over 70 percent of providers state it takes more than one month to collect outstanding payments from patients, and they expect to recover only 50 to 70 percent of the balances due. - Value-based care and shrinking reimbursements require overhead reduction and well-honed workflows.
Providers need efficiency gains in every aspect of healthcare operations. McKinsey reports improving back-end efficiency and effectiveness from average- to top-quartile levels can increase a healthcare system’s net margin by 2 percentage points.For ambulatory practices, an efficient back-office is also critical to the bottom line. The time clinicians spend on administrative versus clinical duties can add up to more than 50 percent of practice losses. If clinicians are handling billing issues instead of caring for patients, they are not driving revenue. - Patients now place more demands on providers when it comes to their healthcare.
From expectations of pre-visit cost estimation to online payment portals, patients want their healthcare experiences to be more like the ones they receive from high-end retailers.
Patients’ expectations for the back office now rival their high standards for front desk and clinical staff. They want the entire care experience to be hassle-free from booking the appointment to paying the bill.
Today’s patients want:
- To understand the cost of service BEFORE booking an appointment.
- To receive bills and statements via their preferred communication channel, be it postal mail, email or text message.
- A wide range of payment options. According to the 2017 Black Book survey, patients pay almost 62 percent of medical bills online, and 95 percent of patients writing checks would pay online if a payment portal existed.
Technology to the Rescue
Transitioning away from paper communications and manual billing reconciliations could save the healthcare industry billions of dollars. According to the same Black Book survey, 83 percent of providers will look to technology for the answer to manual, error-prone processes.
Innovative revenue cycle management (RCM) and payment processing companies know that patients who are engaged throughout the service delivery cycle are more likely to participate fully in billing and payment processes. With RevSpring, you can leverage data-driven patient engagement programs and intelligent communication workflows to create tailored pathways. The analytics-powered paths drive patients to take charge of their bill payments and care schedules.
In addition to assisting organizations with optimized statement printing, our predictive analytics enhance automation efficiencies and payment collection rates. From automating payment channel preferences to customizing outbound interactive voice response systems, you can engage patients and power payments with Intelligent Workflow Solutions.
Learn more about patient engagement and automatic payment reconciliation by contacting learnmore@revspringinc.com.