- Display graphical messaging, prioritized and applied dynamically for each patient
- Track communication performance against your business goals
- Drive action and measure performance for multiple desired outcomes (payment plans, eStatement delivery adoption, mobile payment adoption, and patient portal adoption for meaningful use, among others)
- Change messages in real-time based on history, real-time decisioning, and predictive modeling to influence patient actions taken
- Change payment behavior across all touch points, including the patient payment portal
- Automate outbound workflow action in the communication channels patients are most likely to engage in
- Support rapid onboarding and statement changes through the configuration engine
- Measure the strength of the whole patient engagement program with A/B testing to allow for ongoing program optimization
Engagement and Messaging Strategies to Improve Outcomes
Every patient is different. We tailor payment conversation to influence behavior and inspire action. With Vu™ Behavioral Insights, health systems’ communications and payment options are hyper-focused on each patient, using multi-channel outreach to highlight the unique payment pathways that are best for them.
RevSpring works with each client individually to establish goals or desired outcomes based on their strategic business objectives. From there, we dynamically align messaging and payment strategies to patients based on what we know about them to achieve the desired results. Our best practice designs can help health systems target specific self-pay revenue cycle improvements, such as speed to payment, online adoption, payment plan utilization, bad debt reduction, and overall cost optimization.
Predict Payment Outcomes So You Can Improve Them
Use your patients’ behavioral, financial, and demographic patterns and preferences to predict outcomes and promote the best path to financial resolution for each individual patient, including up-front payment awareness and more appropriate options to pay (pay in full, autopay, payment plans, financing, etc.).
Create a more positive billing experience by giving patients the sense that “you know them” by targeting communications and payment options to their needs, in the channels they prefer to engage in.
- Flexibility to leverage tested, accurate propensity-to-pay modeling
- Demographic modeling does not hit a patient’s credit report and is invisible to the patient
- Financial assistance modeling predicts who is likely to need additional financial counseling early in the revenue cycle and can screen for Medicaid eligibility and route patients into internal workflows accordingly
- Scoring can also drive pre-filled financial assistance applications, available to be signed electronically or mailed directly to pre-qualified consumers
We Know It Works, Because We Continuously Measure It
Vu™ Analytics shows you what to expect from daily, weekly, and monthly patient volumes to maximize collections while maintaining exceptional patient experience. We give your staff at-a-glance dashboards to track patient outreach, propensity-to-pay data, and real-time revenue cycle intel.
- Our custom dashboard allows you to see what’s working, track your key metrics, and optimize your engagement workflows against your goals.
- Identify trends and track KPIs
- Utilize business intelligence, denial analytics, and a custom visual analytics dashboard
- Data integrations with any EHR platform
We Stand By Our Results
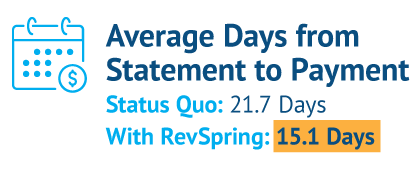
Our relationship managers and analytics teams work together to ensure we are delivering the results we promise. Through Vu, we monitor your results so we can proactively drive adjustments to ensure we’re living up to our promises. This insight into performance against goals helps the business office make intelligent decisions about alternative messaging campaigns, communication strategies, and billing options to optimize results.
- Performance goals established during implementation
- Revenue cycle management assessments
- Implementation services
- Remittance analysis
- Revenue cycle performance recommendations for patient self-pay (both balance after insurance and uninsured populations)
End-To-End Workflow
With the eVoke™ engagement platform, powered by Vu, financial communication is consistent across all touch points —at registration, at the front desk or point of service, via printed billing communications, online, in email and text communications, and over the phone. This type of connected experience will eliminate billing surprises, reduce confusion, boost satisfaction, and strengthen the relationship between you and your patients. By investing in an engagement strategy that clearly demonstrates to your patients that they mean more to you than their balance, you’ll realize unmatched results.
Pre-Service
Gather & Verify Data
Revenue Assurance
Warm to Financial Obligation
Provide Cost Transparency
Facilitate Payment
Point-of-Service
Validate Data
Segment Risk
Identify Financial Obligation
Warm to Financial Obligation
Facilitate Payment
Post-Service
Segment Risk
Resolve Financial Obligation
Personalized Messaging
Automated Billing
Automated Reminders
Facilitate Payment
Follow-Up
Adherence Follow Up
Satisfaction Measure
Follow Up
Appointment
Therapy
Etc.

